East Midlands Ambulance Service (EMAS) has reported a deterioration in ambulance response times and hospital handover delays, with October emerging as one of the most challenging months of the year so far.
The findings are set out in the latest Integrated Board Report ahead of the Trust Board meeting on 2 December 2025, covering every aspect of operational performance, workforce, patient safety and clinical quality.
The data paints a concerning picture for residents across Nottinghamshire and neighbouring counties who rely on fast emergency care, at a time when national targets remain a long way from being met.

The report confirms that ambulance response times for every category of 999 call were slower than planned during October. Category 1 calls – for life-threatening emergencies such as cardiac arrests – averaged 9 minutes 12 seconds against the 7-minute national target, the slowest monthly performance since summer. Category 1 90th percentile times also increased to 16 minutes 15 seconds, further away from the 15-minute national standard. The report’s performance charts show a clear downturn after relative stability earlier in the year.
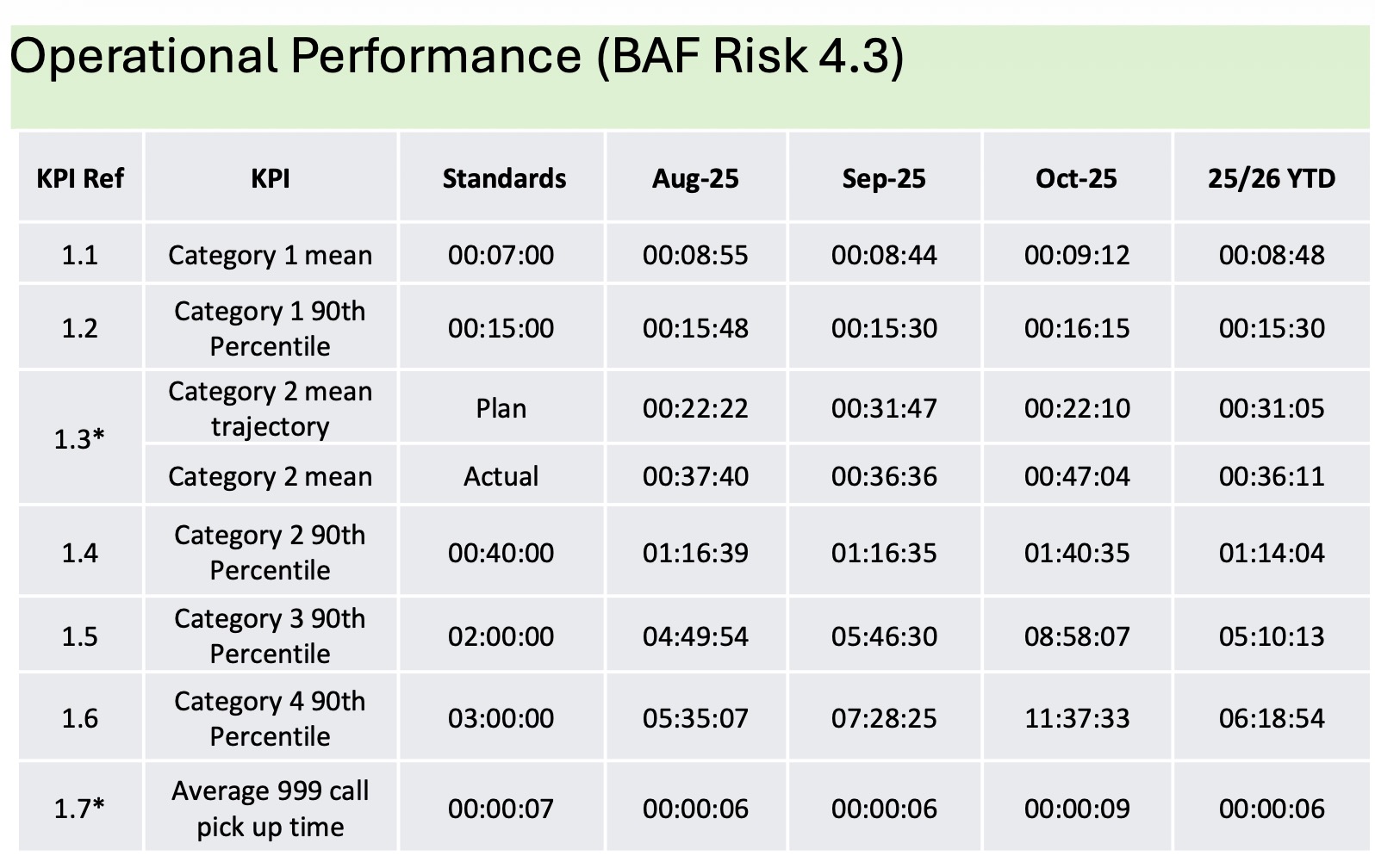
The most serious delays, however, remain in Category 2 calls, which include suspected strokes, chest pain and other serious conditions. These calls make up the majority of EMAS’s workload. October’s Category 2 mean response time rose sharply to 47 minutes 04 seconds, widening the gap between actual performance and the new improvement trajectory set as part of EMAS’s H2 Improvement Plan. According to the performance table on page 5, the plan required a mean of around 22 minutes in October, meaning the service delivered more than double the intended response time.

The 90th percentile for Category 2 calls has also worsened significantly, reaching 1 hour 40 minutes. This brings the East Midlands back into territory previously seen during the most pressured periods of the pandemic, when ambulance queues outside hospitals became a national flashpoint.

The report attributes the decline in response times to a combination of rising incident activity, slightly longer on-scene times and a marked increase in hospital handover delays. Even though Double Crewed Ambulance (DCA) availability was slightly above plan in October, the demand pressures and handover bottlenecks effectively “absorbed” the extra resource, preventing improvements in 999 response times.
Hospital delays remain one of the most critical issues facing EMAS and its patients. October saw an average handover time of 40 minutes 47 seconds, more than 10 minutes above the Trust’s monthly trajectory. The hospital-specific data shows significant variation across the region, with the worst delays occurring locally at Nottingham’s Queen’s Medical Centre (QMC). More than 4,000 hours were lost at QMC alone in October due to prolonged pre-handover waits, the highest level across all regional hospital sites. Leicester Royal Infirmary recorded over 3,500 lost hours, while Royal Derby Hospital exceeded 2,100.
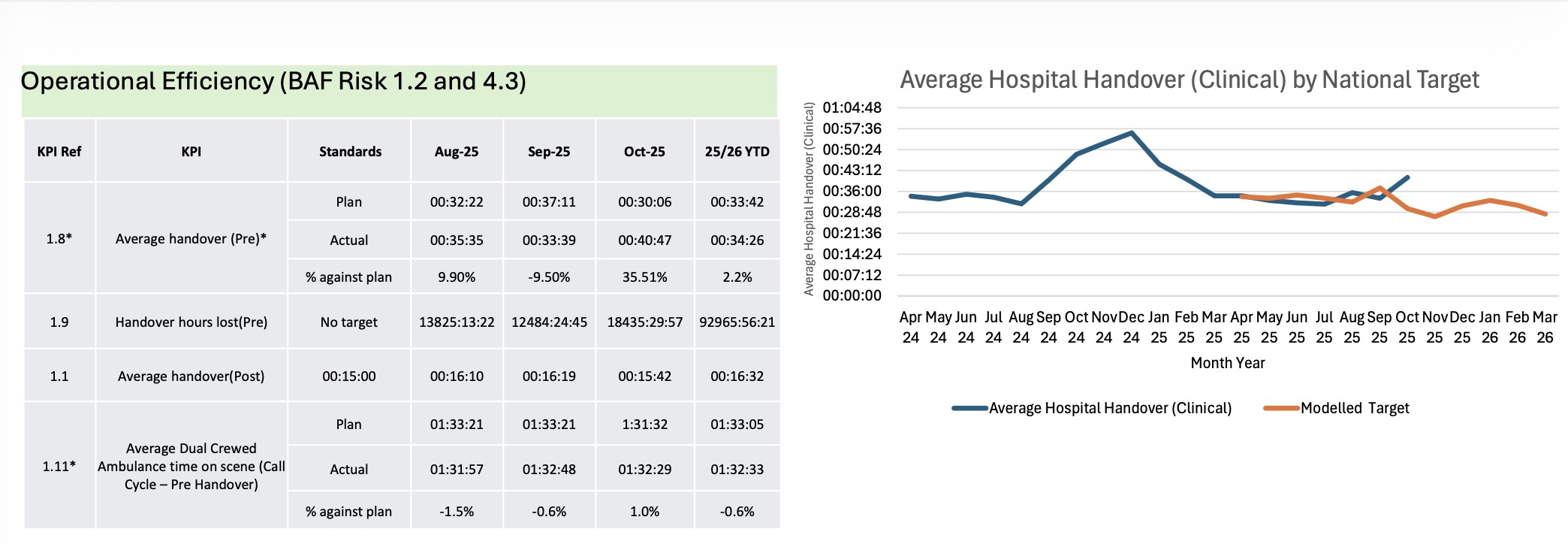
Almost a quarter of all ambulance handovers across the East Midlands took more than 45 minutes in October. At QMC, 46% took longer than 45 minutes, which is nearly double the regional average. Across the region, more than 6,500 patient handovers exceeded one hour, including more than 1,500 at QMC and over 1,200 at Leicester.
The scale of these delays is also illustrated through lost staffing time. According to the narrative on page 6, handover delays greater than 15 minutes in October equated to just over 1,500 12-hour ambulance shifts, equivalent to an average of fifty crews a day tied up waiting outside hospitals rather than responding to patients.
The pressures have also carried through to the Non-Emergency Patient Transport Service (NEPTS), which covers Derbyshire, Lincolnshire and Northamptonshire. High discharge activity, short-notice bookings and increasing numbers of high-acuity and stretcher-dependent patients, particularly in Lincolnshire, contributed to longer waits for same-day discharges. While some renal patient KPIs were met consistently (with 94% collected within 80 minutes), other measures such as timely discharges two hours after the booked collection time remained well below the 90% standard, holding at 47% for the month.
Workforce availability continues to affect operational performance. Sickness absence reached 6.89% in October, above the Trust’s 6.05% target, although still an improvement on last year’s 7.76%. Year-to-date sickness sits 0.70% above plan. The report confirms ongoing focus on attendance management, wellbeing and local leadership to bring figures down. Staff turnover remains stable and low at 7.57%.
However, both appraisal completion and essential training compliance remain below required levels. Frontline appraisal compliance has slipped to 73%, with a target of 95% by March 2026. Mandatory training for frontline staff stands at 77%, well below the 85% target. Non-frontline training compliance is performing much better, reaching 93% in October.
The quality section of the report shows incident reporting levels remain within expected ranges, with 822 IR1 incidents logged in October. Ten patient safety investigations were initiated during the same month. Two validated eight-hour delays in Emergency Departments were recorded, both at a single acute trust within a 24-hour period. So far, no collaborative harm reviews have been requested for these cases, although the report warns that a lack of system-wide review risks missing opportunities to learn from these extremely long waits.
Clinical quality indicators remain mixed. While the resuscitation bundle performance is above the national average, STEMI care bundle compliance remains below the national benchmark. Falls care bundle performance is notably low, with EMAS scoring 22.8% in the most recent national publication compared to the national average of 43.3%. The narrative on page 14 notes that the most common reason for failing the falls care bundle is incomplete documentation of the patient’s history of falls.
For local residents, the combined impact of rising response times, extended hospital waits and ongoing workforce challenges means continued pressure on emergency services heading into winter. Patients experiencing stroke, chest pain or severe illness are likely to wait significantly longer than national targets, and in some cases much longer than the new internal improvement targets EMAS has set for itself.
The service stresses that it is working with hospital trusts and system partners to reduce handover delays and improve performance, but the October data underscores the scale of the challenge. The Trust Board is being asked to take assurance from the report, but it is clear that the gap between current delivery and national standards remains wide.

Public concern about ambulance delays has remained high across the East Midlands for several years, particularly following the extreme pressures of winter 2022–23, when long queues outside hospitals became a highly visible symptom of wider NHS strain. While EMAS has made gradual improvements during quieter months, the October figures suggest performance is once again deteriorating as winter demand builds.
The Board is expected to discuss these issues in detail on 2 December and review progress against the H2 Improvement Plan, which aims to bring Category 2 response times back within the national 18-minute target by the end of the 2025/26 financial year. Based on current performance, significant improvements in hospital flow, staff availability and triage capacity will be needed to achieve this.